|
Many couples faced with infertility are still unable to become pregnant after first line therapy such as ovulation induction, intrauterine insemination, or reproductive surgery. For these couples, the logical next step is to explore the Assisted Reproductive Technologies (ART).
These treatments include In Vitro Fertilization and other assisted laboratory techniques designed to improve fertilization. Compared to simpler treatments, ART procedures typically have very high success rates but are more complex as they involve well-coordinated, perfectly timed effort between the medical team, laboratory staff and the patient.
Couples who are aware of all aspects of their treatment will be more co-operative since they know exactly what to expect and when. Most importantly they are fully informed on issues such as success rates of the treatment, complications and possible side-effects. |
| IVF Medications |
|
It is necessary to take certain medications during the IVF cycle in order to prepare the body for the treatment. The instructions for each medication vary from patient to patient.
GnRH Agonists - Lupride taken as an injection just below the skin and allows the body to produce a greater number of high quality eggs during the treatment cycle. They also prevent the midcycle hormonal surge that can result in the cancellation of a cycle.
Antagonists - Orgalutran and Cetrotide are antagonists of gonadotropin releasing hormone (GnRH) and are used to prevent premature ovulation. These medications are given by injection and the duration of treatment is usually three or four days.
Gonadotropins - Gonadotropins are taken as subcutaneous injections that provide stimulation to the follicles that contain the eggs during the stimulation phase. Gonal F, Recogon, Ovufol HP, Ovugraf HP are the most commonly used gonadotropins.
hCG - hCG is taken as an intramuscular injection and are used to induce the final maturational changes in the eggs and prepare them for retrieval. The most commonly prescribed hCGs are Ovutrig , and Hucog.
Doxycycline - Doxycycline, an antibiotic administered in pill form, is given to the male partner during the wife's stimulation cycle to reduce the low levels of bacteria that may be found in the semen and which may compromise the performance of the sperm during an IVF cycle. It is also given to the female partner to reduce the risk of infection following aspiration of the follicles at the time of egg retrieval.
Progesterone - Natural Progesterone may be taken as a daily intramuscular injection beginning two days after egg retrieval and continuing until the placenta is making adequate amounts of Progesterone. Progesterone can also be given in the form of a vaginal gel or vaginal suppositories or pills. |
| Long Protocol |
|
GnRHa are analogues of gonadotrophin releasing hormone (GnRH) but are several times more powerful. Their administration causes a high output of FSH and LH from the pituitary gland but this is relatively short lasting. Continued administration of GnRHa depletes the pituitary stores of these hormones and their output falls tovery low levels. This is called pituitary downregulation and the lack of response of the pituitary gland to further doses of GnRHa is said to be due to pituitary desensitization. These events are usually completed with 10-14 days of starting GnRHa administration.
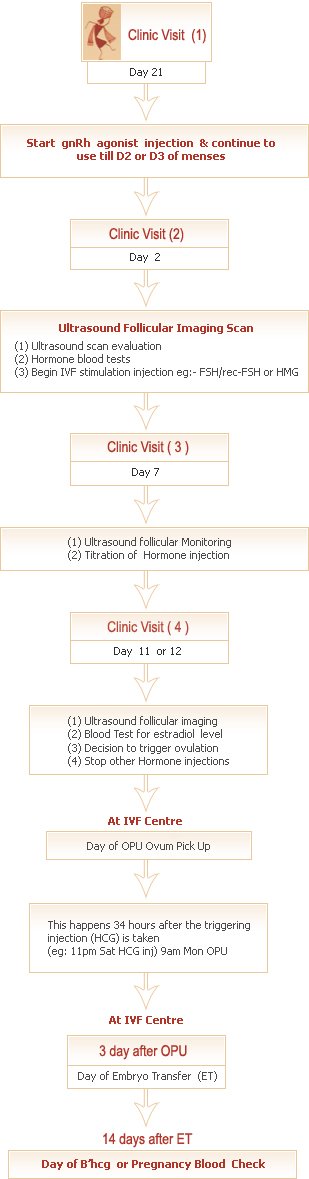
Long protocol GnRHa administration is commenced from either the midluteal phase (Day 21) of the menstrual cycle preceding the treatment cycle or from the early follicular phase (Day 2) of the treatment cycle itself. The GnRHa is administered for 10-14 days before commencing the injection of gonadotrophins and continued until the administraton of the ovulation trigger. |
| Long Protocol |
|
 |
| |
|
| Short Protocol |
|
This is a quick and patient friendly approach to IVF management.
Here, the number of days of IVF stimulation are much reduced and the dosage of the drug used may also be lower. To prevent the brain from secreting LH (Luetinizing Hormone) which can cause damage to the developing follicles, an injection called
GnRh antagonist is offered daily.
This protocol is especially useful for older women, Poor responders in previous IVF cycles, women with PCOS etc. The risks by hyperstimulation syndrome with this protocol is reportedly much lower in these PCOS subgroups.
Over all pregnancy rate are similar with both the “long protocol” and "short protocol” |
| Short Protocol |
|
 |
| |
|
| SuperOvulation |
|
Ovarian stimulation for IVF treatment aims for multiple follicular development and the retrieval of many oocytes. It is believed that the chances of conception are improved by the transfer of more than one good quality embryo into the uterine cavity.
The dose of gonadotrophin injection administered to any particular patient depends on factors such as age, build, dose used in previous treatment cycles. Whether the ovaries are polycystic, history of ovarian hyperstimulation syndrome (OHSS) in a previous treatment cycle and ovarian or periovarian surgery. The dose may have to be increased or decreased depending on her response to the administered drugs. Some patients may receive 100-150IU a day while other will receive 225IU or more. A successful treatment outcome becomes less common when more than 450 IU are required each day especially when there is evidence of incipient ovarian failure in the pre-treatment period. Gonadotrophin injections are continued until many of the developing follicles attain the diameter of 18-22mm. The injections are usually given for a total of 12-16 days administration can be extended to 21 days for poor responders or when there is a very cautious approach to superovulaton, for example, in those who had previous OHSS or are known to have polycystic ovaries. |
| Ovulation Trigger |
|
| Since the natural LH surge is abolished by the use of GnRHa, alternative ovulation triggers are required. The LH surge initiates final maturation of the oocytes and softening of connective tissue elements that anchor the oocytes - cumulus complex (OCC) to the wall of the follicle. The latter change make it easier of r the OCC to become dislodged at the time of ovulation or oocytes aspiration. Human chorionic gonadotrophin (hCG) is a glycoprotein hormone that shares key structural similarities with LH and can induce similar oocytes maturation in developing follicles. An injection of 5000-10000 IU of the drug is administered when the developing follicles reach the required size. The oocytes are aspirated from the ovaries about 34 - 36 hours after the hCG injection. |
| Patient Monitoring During IVF Cycle |
|
Ultrasound scanning is the main method of monitoring the woman's response to ovarian stimulation. Most of the scanning will be carried out transvaginally because this gives the best image of the pelvic organs as it allows the use of higher ultrasound frequencies.
An initial ultrasound scan is carried out 10-14 days after commencing GnRHa treatment. The endometrial lining is examined to make sure it is thin and normal. The endometrial thickness is preferably less than 3 mm and should not measure more than 5 mm. The ovaries are carefully examined to exclude cysts or any other abnormalities. As noted earlier in this chapter the initial flare-up of FSH and LH production after commencing gonadotrophin administration. Alternatively the GnRHa can be continued until the cyst disappears before commencing gonadotrophin administration.
The Next ultrasound scan will be scheduled to take place after six to eight days of gonadotrophin injections. Subsequently, scans are carried out daily, every other day or at longer intervals depending on the observed patient response. On each occasion the ovaries and uterus are examined. The number of developing follicles in each ovary is checked and their size measured. The endometrial thickness and reflectivity are assessed and noted.
The concentration of oestrogen, progesterone, FSH and LH may be measured through blood tests that are carried out 10-14 days after commencing GnRHa treatment. This is to ensure that adequate controls has been achieved over pituitary function. Subsequent hormone assays measure mainly oestrogen which is produced by the developing follicles in the ovaries. The concentration of this hormone in blood can give an indication of how well the ovaries are responding the stimulation and whether the woman is over responding to the gonadotrophin injections. It may be useful to include LH as one of the treatment cycle of the hormone. |
| Ovum Pick up (OPU) |
|
Patient reports to the IVF centre early morning after having fasting overnight.
She is prepared in the ward and taken to the procedure room of the unit.
Various forms of anaesthesia can be used but short-acting intravenous sedatives and narcotics are popular. The vagina can be cleansed with antiseptics and irrigated with normal saline to remove traces of the antiseptic.
A transvaginal ultrasound scan is carried out and oocytes are aspirated from follicles in both ovaries through a needle that is used to pierce the vaginal wall and puncture the follicle. Each tube of aspirated fluid is examined under magnification to identify the oocytes which is then removed and washed in clean culture medium. The retrieved oocytes are placed in culture dished containing culture medium and kept in an incubator that is maintained at 37degree C and having an internal atmosphere of 5-6% CO2 in humidified air.
Transvaginal oocytes collection is a relatively safe procedure. The patient should feel no pain and regain full consciousness soon afterwards. The procedure takes an average of 30 minutes. After a short while in the ward, the patient is usually discharged home on that same day. Before discharge the findings at operation are discussed with the couple and they are informed of the number of oocytes that were collected. |
| Semen Collection on Day of OPU |
|
The patient's partner is required to produce a semen sample. This can be carried out at the same time the oocytes collection is being performed.
The semen sample is generally produced by masturbation following two to three days of obstinence from ejaculation. The quality of the semen sample may become poor if the period of abstinence is more 7-10 days. The ejaculate is collected into sterile plastic containers which are non - toxic to spermatozoa. It is recommended that the man washes his hands and genitals with soap, rinses them several times with clean water and dries with a clean towel. No lubricant such as petroleum jelly is allowed during masturbation to avoid problems of toxicity to spermatozoa.
The semen sample is analysed and then prepared for IVF. Different methods of sperm preparation are in use. All methods aim to remove seminal fluid and its chemical constituents, dead and abnormal spermatozoa and other cells from the sample thereby leaving only normal motile spermatozoa suspended in clean culture medium. |
| Progestrone Supplementation |
|
Progesterone supplementation is started in the evening, following oocytes collection or the day after.
Insertion of the pessaries is continued until the pregnancy test result is available. If negative, she stops inserting the pessaries; the menstrual period should of rt within two weeks. If the patient becomes pregnant she continues with progesterone supplementation until 12 weeks of pregnancy. |
| Number of Embryos Transferred |
|
It is realized that the chance of pregnancy occurring in any particular patient partly depends on the number of embryos transferred. The more the number of embryos that are transferred the greater the chanc4s of conception, at least up to a certain point. However, the incidence of multiple pregnancy also increases with the number of embryos that are replaced.
A compromise which many clinicians generally adopt is to transfer three embryos. Young patients (early to mid-twenties) who are deemed suitable may be advised, but not coerced in any way, to have only two embryos replaced. It is also advisable for females below 35 years of age to have on two embryos replaced the first time they have IVF treatment, provided all other aspects of their treatment are normal. Three embryos may be transferred in women between 36 and 40 years while four embryos may be transferred in women above 40 years, especially if they have had previous unsuccessful treatment. Both the patient and the medical tam have to decide on how many embryos to transfer and the patient has the final say on this matter. |
| |
Table Transferred embryos number and its relationship to pregnancy and
multiple pregnancy rates |
|
|
Number of Transferred
Embryos |
Pregnancy
rate (%)
|
Single (%) |
Twin (%) |
Triplet or
more (%) |
|
|
| 1 |
10 |
>99 |
<1 |
Rare |
| 2 |
25-30 |
74 |
25 |
1 |
| 3 |
30 |
70 |
24 |
5-8 |
|
| |
|
| Embryo Transfer |
|
| Embryo transfer is usually simple and straightforward. It is not a painful procedure. The women is positioned appropriately and a vaginal speculum inserted so that the cervix is seen. The cervical os is gently wiped with cotton wool balls moistened with normal saline and then culture medium. At times a pair of vulsellum forceps is applied on the cervix to stabilize it and straighten the angel between the cervical canal and the axis of the uterine cavity thereby making embryo transfer easier. The embryologist picks up all the embryos to be transferred with a thin plastic cannula attached to a syringe and hands over the clinician. The clinician gently inserts the cannula in to the uterine cavity through the cervical os and expels the embryos, with a drop of culture medium. The cannula is then remove, followed by other instruments and the woman left to the lie on the couch for some minutes after which she gets up and goes home. Research has shown that the length of time a woman lies on the couch after the embryo transfer procedure does not affect the subsequent pregnancy rate. |
| Embryo Freezing |
|
Technology is available for cryopreserving embryos.
The pregnancy rate after transfer of frozen-thawed embryos is less than that following transfer of freshly generated embryos. However, the availability of frozen embryos increases the pregnancy potential of each IVF treatment cycle; from one episode of oocyte collection a patient may have two to three episodes of embryo replacement with a cumulative pregnancy rate approaching 60% or more. |
| Success Rate of IVF |
|
About 30-40% of women who start each cycle of IVF treatment achieve clinical pregnancies. The success rate depends on several factors many of which are unknown. The known determinants of success include the cause of the infertility, age of the female, the response to ovarian stimulation, semen quality and the number and appearance of embryos generated and transferred.
Conception through IVF and other assisted conception treatments, for a large proportion of couples, is a question of time and the number of attempts. However, everyone, including the medical team, want the treatment to succeed and as soon as possible. This is because of the expensive nature of the treatment, the risk of injury during and after the treatment, associated stress and disruption of the couple' routine and work. |
| Complications of IVF |
|
IVF treatment is expensive and may drain the financial resources of infertile couples. It also imposes a strain on the physical state of the woman and the couple's mental state. Minor side-effects of administered drugs and hormones include headaches. Those who sniff GnRHa preparations may have nasal problems arising from irritation of the mucousme membranes. There may be allergic reactions to some the injections. The injections may be painful and cause localized skin skin reactions including bruising and redness. Some IVF treatment cycles may be cancelled prior to the stage of oocytes collection. The incidence varies but up to 10-15% of treatment cycles can be cancelled. This is usually due to poor response to ovarian stimulation with the number of developing follicles being less than three. Occasionally it may be due to a very excessive response which could become life threatening of hCG is administered and oocyte collection with subsequent embryo transfer is carried out. Premature surging of LH production by the pituitary gland used to be a common cause of cycle cancellation but this is much less common nowadays that GnRHa is being used to suppress pituitary function using the long protocol in major proportion of patients.
Cramping pain just like 'period time pains' may be felt after oocytes retrieval. This may last for 24-48 hours. There may be slight bleeding from the needle punctures in the vaginal following oocytes collection Occasionally the bleeding may be heavy and require haemostatic sutures on the vaginal wall. A blood vessel may be punctured and bleed inside the pelvis. Bowel loops can also be punctured. This incidence of infection is low; 0.58% has been quoted by some researchers. There is always a chance that none of the oocytes will become fertilized by the sperm. This fertilization failure is mainly due to sperm defects although poor oocytes quality can be implicated at times.
Ovarian response to stimulation may be excessive with the ovaries becoming very enlarged with fluid accumulation in the abdominal cavity. In severe cases, there may be fluid accumulation around the heart and lungs (pericardial and pulmonary effusion respectively).
Abdominal distension and discomfort are early symptoms and the patient may become very sick and in need of hospital admission and treatment. This OHSS and is potentially life threatening in the severe variety. The mild type of is present in about 10-25% or more of patients who have IVF treatment. All that is needed is bed rest with increased oral intake of fluid and the use of mild analgesics such as paracetamol. The moderate type OHSS occurs in less than 5% of patients while the incidence of the severe type is 1-2%.
The incidence of multiple pregnancy is high because more than one embryo is transferred in order to improve the chances of conception. The incidence of twin pregnancy is 25% and triplets 5 % when three embryos are transferred. Quadruplets and higher order gestations are possible because one or more of the three transferred embryos may each divide into two.
This is also the reason why a patient who has only one embryo transferred can still have twins and the woman who had two transferred in have triplets.
Ectopic pregnancy is more common after IVF treatment than in the normal population but no one knows exactly why this is so. It may relate to the fact that more women who have IVF treatment have tubal problems which predispose them to having ectopic pregnancies. The incidence of ectopic pregnancy after IVF treatment is approximately 3% of all pregnancies.
About 25% of IVF pregnancies may miscarry. Initially this incidence appears to be high but studies in the general population indicate a similar miscarriage rate. However, some women, such as those who have polycystic ovary syndrome, have a higher miscarriage rate than others, irrespective of whether they conceive naturally or though IVF treatment. |
| IVF Babies |
|
Babies delivered as a result of IVF treatment and other assisted conception treatments do not seem to have a congenital malformation rate that is greater than that of the normal population. Behaviourally they are similar to other children.
There is no evidence at present two show that their development is different from that of other children and young adults. The first IVF baby, who was born in 1978, is now in her thirties. |
| |